The Welshman on the front line of New York’s battle with COVID-19
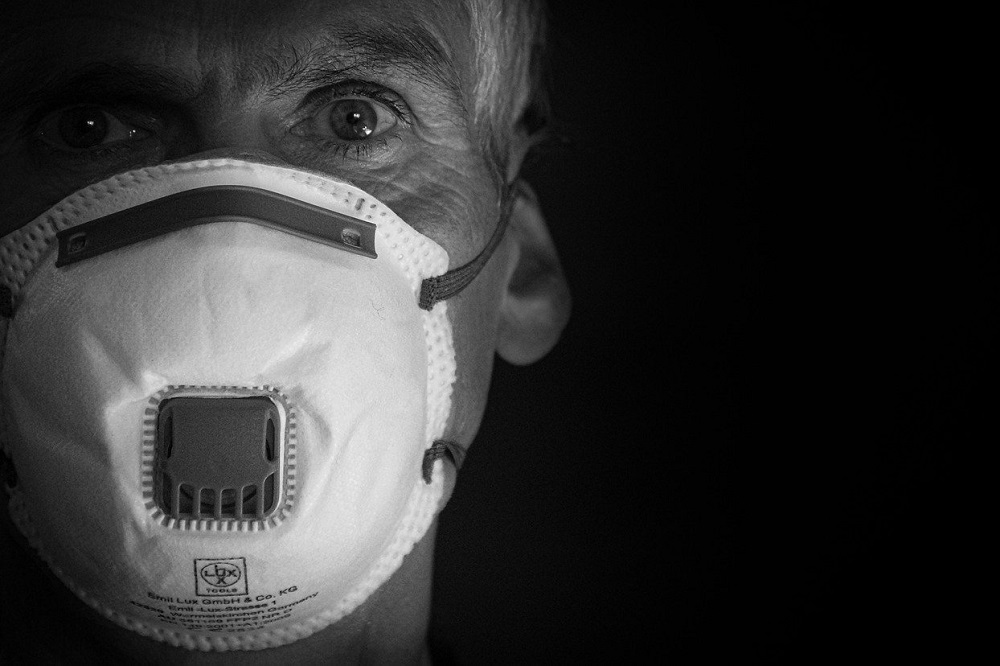
Jaz-Michael King
Friday, April 3rd. It’s been a heck of a week. New York is the hotspot for COVID-19 in the United States and I work for a national public health non-profit headquartered just outside Queens on New York’s Long Island. I moved to New York in 1996, having been born and bred in South Glamorgan. My early years in New York were e-commerce-focused, but since 2001 I’ve worked in health care quality, designing many of the country’s public health care quality reports.
My work is health informatics; I connect data from the sprawling, independent American health sector to state and national health agencies. The team I oversee includes epidemiologists, data scientists, software developers and cloud computing engineers. We create health reporting programs, analytic dashboards, mobile apps for clinical decision support and quality improvement, and various nuts and bolts that help the American health care system keep ticking.
Despite the onslaught of the novel coronavirus the regular work has not slowed, but in addition we’ve been scrambling to respond to the general lockdown by getting our staff kitted out to work from home as well as respond to increasing requests for help from state and federal agencies who are in need of just about everything. Working from home isn’t so easy when you have to connect all those staff back into highly secured health data warehouses, usually not even considered let alone allowed from home offices and unknown devices.
Today I’m trying to source two dozen webcams so the team can huddle to discuss the data, but the cameras are either not available or hugely overpriced. At the same time I’m researching and documenting each state’s Board of Pharmacy to see who has issued what guidelines or restrictions for off-label prescribing to combat COVID-19. Executive orders are pronounced on Monday, altered on Tuesday, rescinded on Wednesday. Things are happening fast.
Hydroxychloroquine
Right now part of the team is engaged with the clinical trials underway in New York to measure the efficacy of Hydroxychloroquine as a treatment for COVID-19. This entails finding COVID positive patients, pulling their medical charts and abstracting the necessary information. To help this effort I’ve been talking with the various health information exchanges; independent repositories of patients’ clinical information with varying degrees of data completeness and connectability. As there are a multitude of electronic health record systems in use I’m trying to narrow down data elements that can be retrieved using something called “FHIR” – Fast Health Interoperability Resources – which would allow me to pull all the data I need from multiple sources into one cohesive dataset for each patient.
Unfortunately, the implementation is not great and I have a range of data that is not connected, or not complete. So, for now, we are working with good old-fashioned paper. Everything is now incredibly time-sensitive; the faster we know something, the more lives we might be able to save.
Along the same lines, as a clinical quality organisation we are concerned about the possibility of adverse drug events from what will be a massive uptick in prescribing drugs “off-label” to treat the disease, and the drugs in question come with a litany of contraindications and considerations – so my software team is rapidly developing an app to put the relevant risk assessment and guidance in the hands of prescribers wherever they may be, which at this point in New York includes hospitals, clinics, a convention centre, a Navy hospital boat that arrived a couple of days ago, and this week we’ll add a tennis centre and a cruise ship terminal as alternate care facilities.
Overwhelmed
As the phone lines are overwhelmed by millions of New Yorkers now working from home, we need to make sure it can work in an offline mode but push the most current guidance, regulations, executive orders and restrictions to each device as soon as possible. Despite liability waivers, no-one wants to cause undue harm to their patients, so it will be vital to disseminate the peer-reviewed science as quickly as possible to as many people as possible.
Prescribers who are in the field hospitals, in the tents, generally cut off from their usual health record system will need accurate guidance on treatment and follow-up. So we’re working to have that done early next week.
Saturday, April 4th. Day by day the numbers are getting bigger. Every afternoon I review mortality data, new case counts, number of discharges. Every night I review hospitalisations across New York City, New York State, and the United States. Every morning I review emergency management dashboards, and am reminded that my blinkered corner of the response is tempered by other factors: issues with the utility companies, refrigerated trucks pre-positioned to serve as ad hoc morgues to handle the unprecedented number of corpses, New Yorkers having to watch bodies being forklifted into containers on the street. We’re simply out of room.
The Greater New York area is home to over 20 million people. I grew up in Llanilltud Fawr, 6,000 people back then. The numbers here can be staggering.
Hospitals are running out of ICU beds and ventilators – half the hospitals in NYC have none left – but the disparate systems and companies make it difficult to transfer patients from the hospitals that are full to the ones who still have available equipment and healthy staff to operate it. The population density helped the virus spread quickly here, and New York was slower to shut down than say, California. There’s a small respite today. 439 people died of the virus yesterday, a new high for NYC, but the number of new hospital admissions is actually a little lower than expected over the past 36, 48 hours. Maybe we’ve crested that curve, maybe we flattened it a bit earlier than we thought, than our models predicted.
Or maybe it’s just the calm before the storm.
Sunday, April 5th. For now, New Yorkers are taking it in their stride. The New York Welsh are running a virtual pub quiz to replace the regular meetups. The NYC Welsh language learners group has migrated the Sgwrs Cymraeg to Google Hangouts. Outside I can see my neighbour is putting up a fence, albeit with a surgical mask covering his face. Some normalcy remains. Some doesn’t. Conference calls have never had quite so many dogs barking in the background, as newly-minted home offices have sprung up to accommodate mums and dads told to stay home, alongside the kids and the pets. Child care and lack of school lunches for 1.1 million NYC schoolchildren was one of the reasons NY took a bit longer to close down.
Veterans
It’s almost Sunday evening now and my wife, who is handling a lot of the emergency management for the local hospitals, is trying to connect military veterans’ hospitals with unused beds to the civilian hospitals that are overflowing and begging ambulances to stop bringing them more patients. I suggest we update the 911 system to simply tell people they have a second option; drive to the nearest veterans’ hospital. Does Veterans Affairs even have ambulances? Questions we never before needed the answers to are needed five minutes ago. All days are workdays now, and they all feel the same. Friday feels like Tuesday, Sunday feels like Friday. Scheduled calls start at 8am and carry on into the evening, aloof about what day it is or isn’t.
I’m nervously awaiting updated reports, and planning the week’s activities assuming we hit peak hospital census in the next few days. People I need to talk with might not be available by Wednesday. My staff who have newfound childcare issues may not be as ready to respond as I’d like.
I meet with some of the staff who want to see what we might learn from patients who were already on Hydroxychloroquine for other reasons. We have a huge amount of data from health care billing claims that might let us compare mortality rates in persons taking the drug versus those not. People with Lupus may already be taking the medication, and we know they are getting COVID-19, so what can we learn about that segment of the population? Are they faring any better or worse in any statistically significant fashion? Tomorrow we will explore the billing and prescribing data and see how useful it might be.
Bills
Out of the corner of my eye, I see an update from the State of New York’s health commissioner relaxing rules on reviews for medical necessity and issuing guidance to the state’s health insurance companies, who are going to be getting a lot of new bills for their insured members. It’s not urgent, I’ll read it in full later. But it bears reminding: at some point a lot of COVID patients are going to get very large, very surprising bills for the out-of-network care they received during the pandemic. An emergency room visit can be several thousands of dollars here in New York. Not too many people are thinking about that issue, yet.
Tonight I need to think about ways to mitigate the five-figure telephone bill my staff are running up now that they’re all calling into meetings instead of using the office lines and equipment. The dog, who has no such concerns, wants to go outside, and having no reason to do otherwise, I let him.
Support our Nation today
For the price of a cup of coffee a month you can help us create an independent, not-for-profit, national news service for the people of Wales, by the people of Wales.





Phew!
Fascinating journalism from global sources. Nation Cymru is coming of age. Gwaith gwych bawb.
Diolch for writing this. A fresh, excellent story about a tragic story. Cymru am Beth,and Go New York City, New York State and the world.